Select Endpoints From TRUE NORTH
The primary endpoint was clinical remission at Weeks 10 and 52. Key secondary endpoints included clinical response, endoscopic improvement, endoscopic-histologic mucosal improvement (EHMI) at Weeks 10 and 52, and CS-free clinical remission at Week 52.1 For full study design, click here.
TRUE NORTH Induction Data
Week 10
Post-hoc Analysis:
Symptomatic Response
Clinical
Response
Clinical
Remission
Endoscopic
Improvement
EHMI
POST-HOC ANALYSIS: SYMPTOMATIC RESPONSEa OBSERVED IN PATIENTS TREATED WITH ZEPOSIA AS EARLY AS WEEK 2—1 WEEK AFTER COMPLETING THE 7-DAY DOSE TITRATION1-5
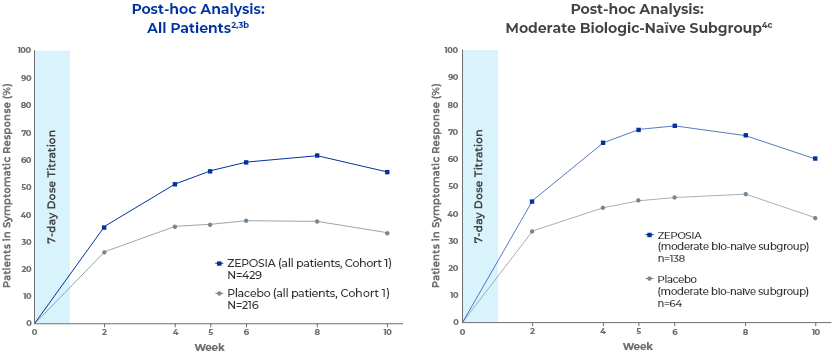
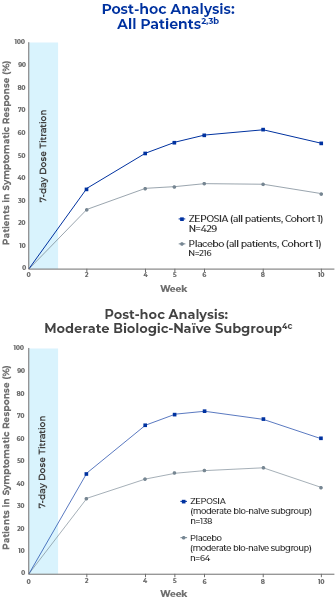
In a post-hoc analysis, patients treated with ZEPOSIA observed a decrease in RBS and SFS as early as Week 2, 1 week after completing the 7-day dose titration.1,3
- Efficacy analyses in the moderate, biologic-naïve subgroup were not prespecified.4
- aSymptomatic clinical response is defined as a decrease from baseline in the combined 6-point SFS + RBS by ≥1 point and >30%, and a decrease of ≥1 point in RBS or an absolute RBS of ≤1 point.2,5
- bData are based on the nonresponder imputation.2
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
RAPID CLINICAL RESPONSE WAS OBSERVED AT WEEK
10 IN THE ALL-PATIENTS GROUP1a
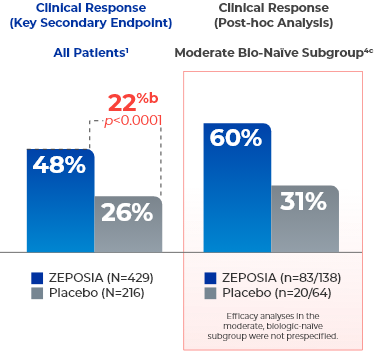
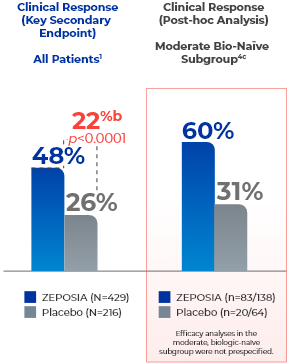
- aClinical response is defined as a reduction from baseline in the 3-component Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of 0 or 1.1,4
- bTreatment difference (adjusted for stratification factors of prior TNFi exposure and corticosteroid use at baseline).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
Post-hoc analysis:
49% of nonrespondersd who entered the open-label extension at Week 10 after the
induction period observed symptomatic clinical response by Week 20e (open-label extension
Week 10)6
- Symptomatic clinical response is defined as a reduction from baseline in the partial Mayo score of ≥1 point and ≥30% and a ≥1-point decrease in RBS or absolute RBS ≤1.2,5
- Efficacy analyses of symptomatic response were not prespecified.
- dNonresponders were patients who did not achieve clinical response (defined as a reduction from baseline in the 3-component Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of 0 or 1) on ZEPOSIA at Week 10 of induction and entered the OLE.1,6
- eData are based on the nonresponder imputation.6
EHMI=endoscopic-histologic mucosal improvement; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
CLINICAL REMISSION WAS OBSERVED AT WEEK 10
IN THE ALL-PATIENTS GROUP1a
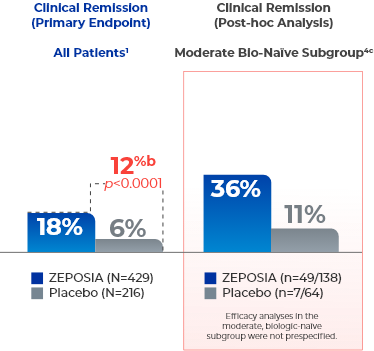
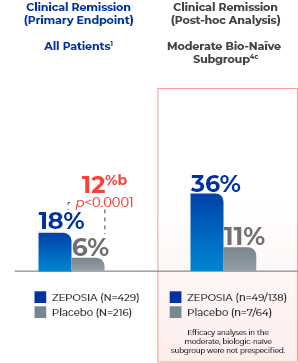
- aClinical remission is defined as RBS=0, SFS=0 or 1 (and a decrease of ≥1 point from baseline SFS), and endoscopy subscore=0 or 1 without friability.1,4
- bTreatment difference (adjusted for stratification factors of prior TNFi exposure and corticosteroid use at baseline).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
ENDOSCOPIC IMPROVEMENT OBSERVED AT
WEEK 101a
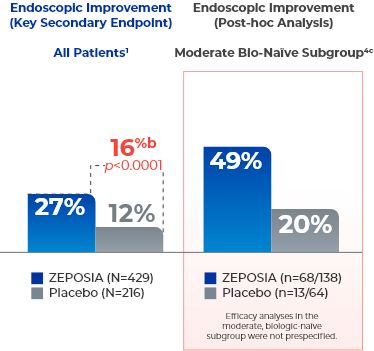
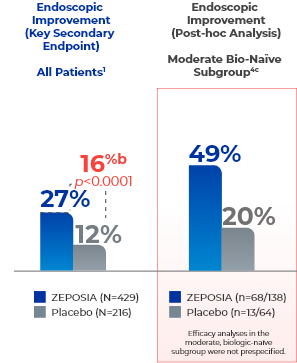
- aEndoscopic improvement is defined as a Mayo endoscopy subscore of 0 or 1 without friability.1,4
- bTreatment difference (adjusted for stratification factors of prior TNFi exposure and corticosteroid use at baseline).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
ZEPOSIA DEMONSTRATED MUCOSAL HEALING DEFINED BY SIGNIFICANT
ENDOSCOPIC-HISTOLOGIC MUCOSAL IMPROVEMENT AT WEEK 101a
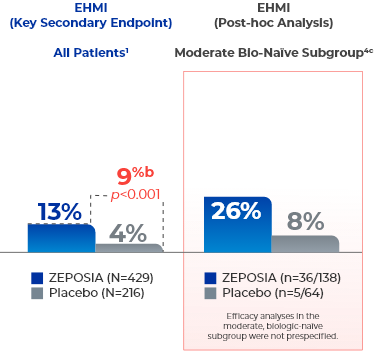
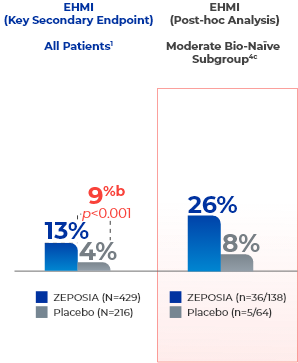
- The relationship of EHMI, as defined in UC Study 1 at Week 10, to disease progression and long-term outcomes, was not evaluated.1
- aEndoscopic-histologic mucosal improvement is defined as both a Mayo endoscopy subscore of 0 or 1 without friability and histologic improvement of colonic tissue (defined as no neutrophils in the epithelial crypts or lamina propria and no increase in eosinophils, no crypt destruction, and no erosions, ulcerations, or granulation tissue, ie, Geboes <2.0).1,4
- bTreatment difference (adjusted for stratification factors of prior TNFi exposure and corticosteroid use at baseline).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
TRUE NORTH Maintenance Data
Week 52
Clinical
Response
Clinical
Remission
CS-Free
Remission
Endoscopic
Improvement
EHMI
CLINICAL RESPONSE INCREASED AT WEEK 52 IN THE ALL-PATIENTS GROUP1a
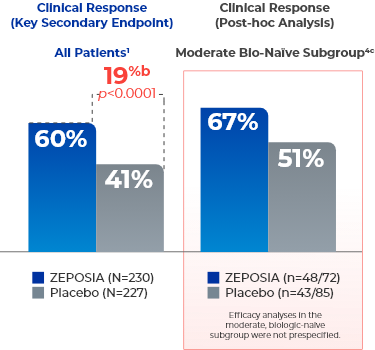
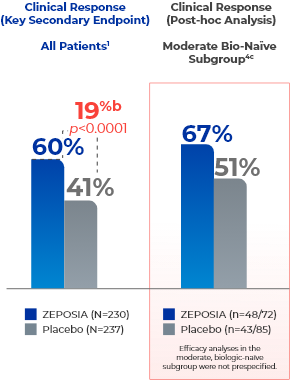
- aClinical response is defined as a reduction from baseline in the 3-component Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of 0 or 1.1,4
- bTreatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at Week 10).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
CLINICAL REMISSION WAS SUSTAINED AT WEEK 52 IN THE ALL-PATIENTS GROUP1a
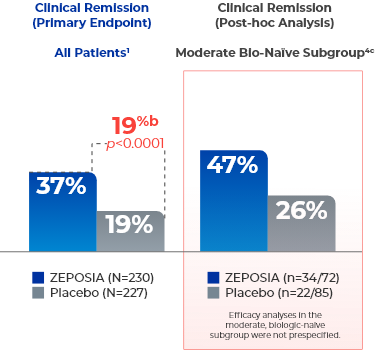
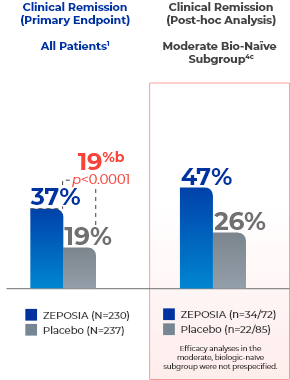
- aClinical remission is defined as RBS=0, SFS=0 or 1 (and a decrease of ≥1 point from baseline SFS), and endoscopy subscore=0 or 1 without friability.1,4
- bTreatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at Week 10).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
CS-FREE REMISSION OBSERVED AT WEEK 52 IN THE ALL-PATIENTS GROUP1a
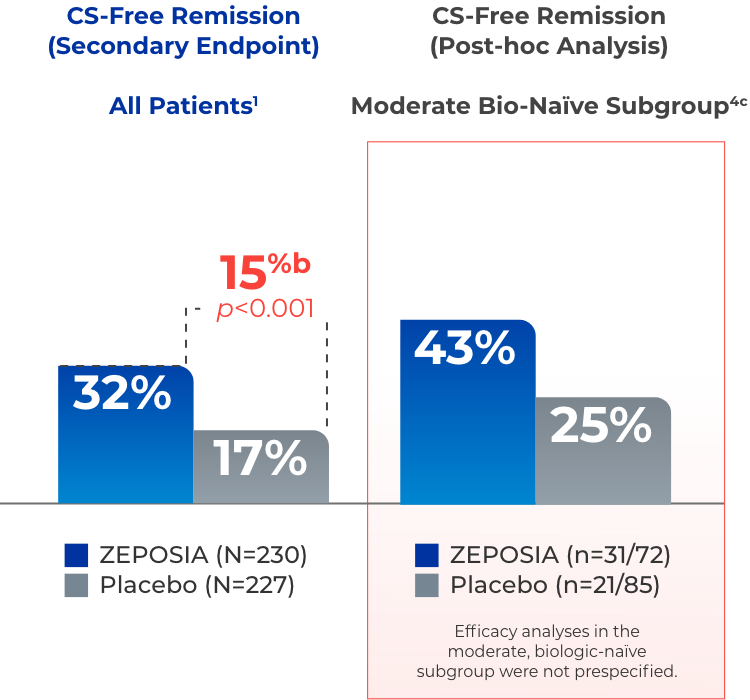
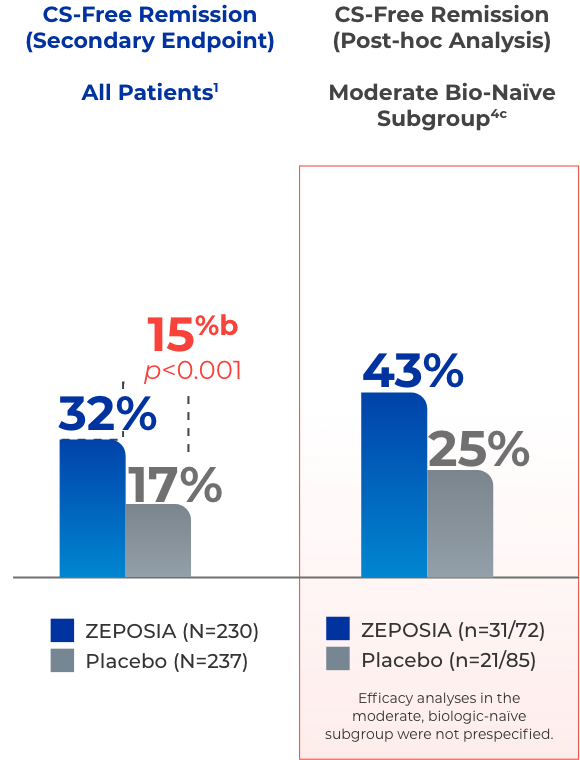
- aCS-free remission is defined as clinical remission at Week 52 while off corticosteroids for ≥12 weeks.1,4
- bTreatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at Week 10).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
ENDOSCOPIC IMPROVEMENT OBSERVED AT
WEEK 521a
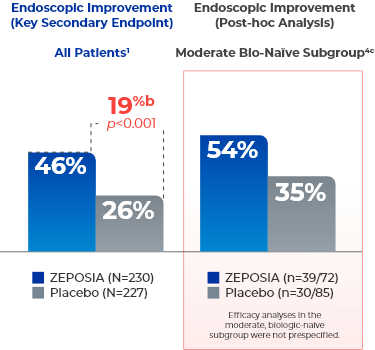
- aEndoscopic improvement is defined as a Mayo endoscopy subscore of 0 or 1 without friability.1
- bTreatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at Week 10).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
ZEPOSIA DEMONSTRATED MUCOSAL HEALING DEFINED BY SIGNIFICANT ENDOSCOPIC-HISTOLOGIC MUCOSAL IMPROVEMENT AT WEEK 521a
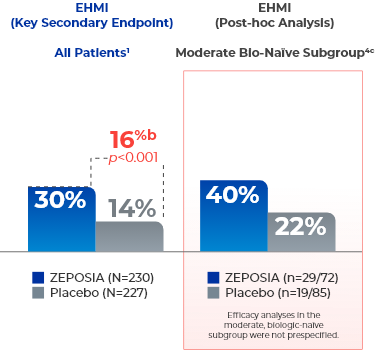
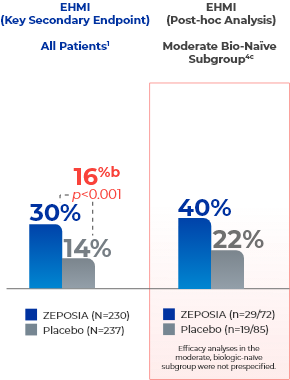
- The relationship of EHMI, as defined in UC Study 2 at Week 52, to disease progression and long-term outcomes, was not evaluated.1
- aEndoscopic-histologic mucosal improvement is defined as both a Mayo endoscopy subscore of 0 or 1 without friability and histologic improvement of colonic tissue (defined as no neutrophils in the epithelial crypts or lamina propria and no increase in eosinophils, no crypt destruction, and no erosions, ulcerations, or granulation tissue, ie, Geboes <2.0).1,4
- bTreatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at Week 10).1
- cModerate biologic-naïve subgroup included patients with a Mayo endoscopy subscore of 2.4
EHMI=endoscopic-histologic mucosal improvement; RBS=rectal bleeding subscore; SFS=stool frequency subscore; TNFi=tumor necrosis factor inhibitor; UC=ulcerative colitis.
TRUE NORTH Open-Label Extension Data, Up to 3 Years
Week 98
(Week 46 of OLE)
Week 146
(Week 94 of OLE)
LONG-TERM RESPONSE, REMISSION, AND CS-FREE REMISSION DATA AT
WEEK 98 (WEEK 46 OF OLE) OF ZEPOSIA, INTERIM EFFICACY ANALYSIS7,8
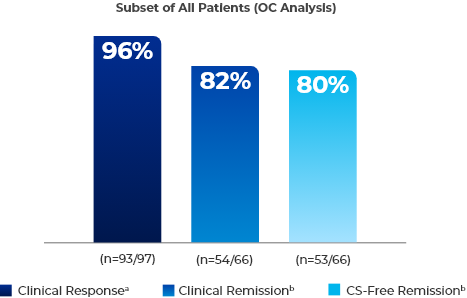
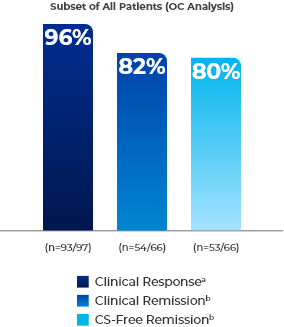
- aSubset of patients in clinical response at Week 52 and had continuous ZEPOSIA exposure (observed case analysis).7
- bSubset of patients in clinical remission at Week 52 and had continuous ZEPOSIA exposure (observed case analysis).8
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9
- In the NRI analysis of a subset of patients in clinical response at Week 52 and had continuous ZEPOSIA exposure, 71% (n=93/131) were in clinical response at Week 98 (Week 46 of OLE) and 56% (n=74/131) were in clinical response at Week 146 (Week 94 of OLE).7
- In the NRI analysis of a subset of patients in clinical remission at Week 52 and had continuous ZEPOSIA exposure, 65% (n=54/83) were in clinical remission at Week 98 (Week 46 of OLE) and 49% (n=41/83) were in clinical remission at Week 146 (Week 94 of OLE).8,9
- In the NRI analysis of patients who were in clinical remission at Week 52 and had continuous ZEPOSIA exposure, 64% (n=53/83) were in CS-free remission at Week 98 (Week 46 of the OLE) and 48% (n=40/83) were in CS-free remission at Week 146 (Week 94 of the OLE).8
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9
- Clinical response is defined as a reduction from baseline in the 3-component Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of 0 or 11,8
- Clinical remission is defined as: RBS=0, SFS=0 or 1 (and a decrease of ≥1 point from baseline SFS), and endoscopy subscore=0 or 1 without friability1,8
- CS-free remission is defined as clinical remission while off corticosteroids for ≥12 weeks1,8
- OLE Study Design
- The TRUE NORTH OLE is an ongoing trial that enrolled participants who were nonresponders at the end of induction, experienced disease relapse during maintenance, or completed maintenance treatment in the phase 3 TRUE NORTH study or remained at study closure and received once-daily oral ZEPOSIA 0.92 mg in the phase 2 TOUCHSTONE OLE. A total of 823 patients from TRUE NORTH entered the TRUE NORTH OLE as of the cutoff date (January 10, 2022).7,10,11 For full study design, click here.
- OLE endpoints were evaluated at Week 46 and Week 94 for a subset of patients who were in clinical remission or clinical response at Week 52 of the TRUE NORTH parent study and who had continuous ZEPOSIA exposure. Endpoints include clinical remission, clinical response, endoscopic improvement, and CS-free remission. Safety was evaluated for all 823 patients who entered the OLE from the TRUE NORTH parent study. Mean ZEPOSIA exposure through the OLE was 2.7 years.7,9,10,12,13
- Data were analyzed in the intent-to-treat population using OC and NRI. OC used the number of patients remaining in the study at the corresponding time point. NRI used the number of patients remaining in the study at the corresponding time point and those who withdrew before the time point but would have reached the time point if they had stayed.9,10
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9,10
CS=corticosteroid; NRI=nonresponder imputation; OC=observed cases; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; UC=ulcerative colitis.
LONG-TERM RESPONSE, REMISSION, AND CS-FREE REMISSION DATA AT
WEEK 146 (WEEK 94 OF OLE) OF ZEPOSIA, INTERIM EFFICACY ANALYSIS7,8
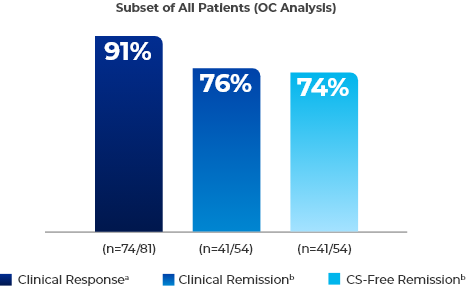
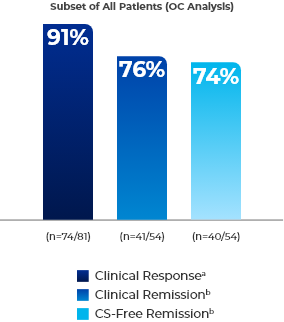
- aSubset of patients in clinical response at Week 52 and had continuous ZEPOSIA exposure (observed case analysis).7
- bSubset of patients in clinical remission at Week 52 and had continuous ZEPOSIA exposure (observed case analysis).8
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9
- In the NRI analysis of a subset of patients in clinical response at Week 52 and had continuous ZEPOSIA exposure, 71% (n=93/131) were in clinical response at Week 98 (Week 46 of OLE) and 56% (n=74/131) were in clinical response at Week 146 (Week 94 of OLE).7
- In the NRI analysis of a subset of patients in clinical remission at Week 52 and had continuous ZEPOSIA exposure, 65% (n=54/83) were in clinical remission at Week 98 (Week 46 of OLE) and 49% (n=41/83) were in clinical remission at Week 146 (Week 94 of OLE).8,9
- In the NRI analysis of patients who were in clinical remission at Week 52 and had continuous ZEPOSIA exposure, 64% (n=53/83) were in CS-free remission at Week 98 (Week 46 of the OLE) and 48% (n=40/83) were in CS-free remission at Week 146 (Week 94 of the OLE).8
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9
- Clinical response is defined as a reduction from baseline in the 3-component Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of 0 or 11,8
- Clinical remission is defined as: RBS=0, SFS=0 or 1 (and a decrease of ≥1 point from baseline SFS), and endoscopy subscore=0 or 1 without friability1,8
- CS-free remission is defined as clinical remission while off corticosteroids for ≥12 weeks1,8
- OLE Study Design
- The TRUE NORTH OLE is an ongoing trial that enrolled participants who were nonresponders at the end of induction, experienced disease relapse during maintenance, or completed maintenance treatment in the phase 3 TRUE NORTH study or remained at study closure and received once-daily oral ZEPOSIA 0.92 mg in the phase 2 TOUCHSTONE OLE. A total of 823 patients from TRUE NORTH entered the TRUE NORTH OLE as of the cutoff date (January 10, 2022).7,10,11 For full study design, click here.
- OLE endpoints were evaluated at Week 46 and Week 94 for a subset of patients who were in clinical remission or clinical response at Week 52 of the TRUE NORTH parent study and who had continuous ZEPOSIA exposure. Endpoints include clinical remission, clinical response, endoscopic improvement, and CS-free remission. Safety was evaluated for all 823 patients who entered the OLE from the TRUE NORTH parent study. Mean ZEPOSIA exposure through the OLE was 2.7 years.7,9,10,12,13
- Data were analyzed in the intent-to-treat population using OC and NRI. OC used the number of patients remaining in the study at the corresponding time point. NRI used the number of patients remaining in the study at the corresponding time point and those who withdrew before the time point but would have reached the time point if they had stayed.9,10
- These analyses were not prespecified and represent a subgroup of all patients from TRUE NORTH who entered the OLE.9,10
CS=corticosteroid; NRI=nonresponder imputation; OC=observed cases; OLE=open-label extension; RBS=rectal bleeding subscore; SFS=stool frequency subscore; UC=ulcerative colitis.

This website is best viewed
using the horizontal display on
your tablet device.

This website is best viewed
using the vertical display on
your mobile device.